The everyday medical risks of street homelessness

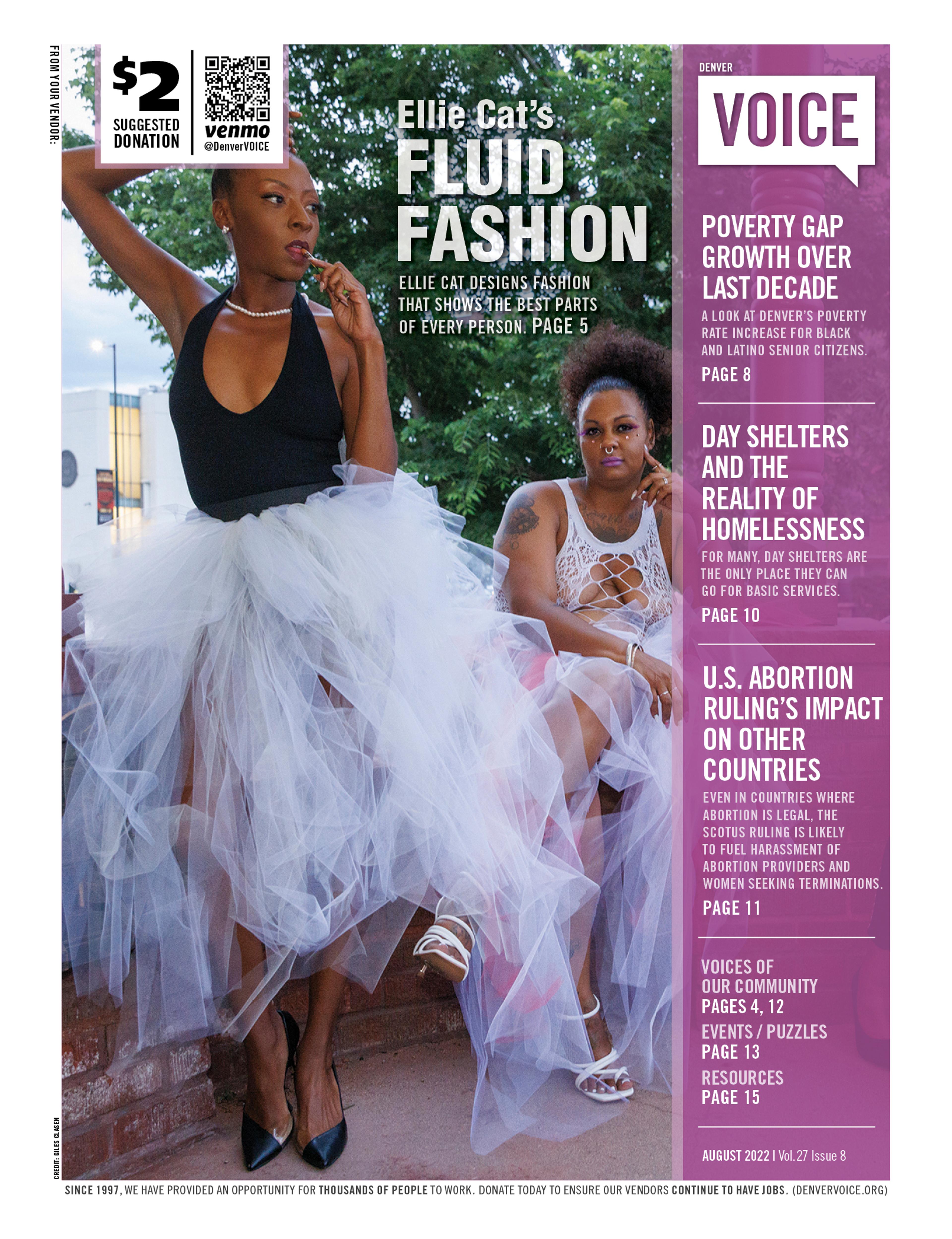
Photos by Giles Clasen
By Giles Clasen
- Lived experience
When Teaya Wrexha woke up near Paco Sanchez Park, her thumb was already swollen to about the size of a squash. She dug into her thumb and began pulling out a bug that had burrowed deep into her flesh.
“I think it was a millipede, maybe a centipede,” she said. “I was sleeping outside, and I woke up with my thumb burning. It was like the thing had gone inside. I squeezed it, and it hurt so bad. I thought I was gonna lose it.”
Living unsheltered means that even a minor wound can become life-threatening. But Wrexha never thought that she was vulnerable to such a “crazy thing”. “It scared me,” she said.
Wrexha tried to clean the wound with what she could find, but she did not have much to work with or any money. She had some antibiotics for dogs, so she took those, hoping that they would help. But her thumb continued to get bigger and bigger until she lay on the grass in agony, sometimes screaming in pain.
Wrexha is transgender but does not take hormones currently. “I found my own gender. I took it back,” she said.
She added that it is difficult to access gender-affirming care while living on the streets, and she is not sure how her body would react to the treatment, so she is waiting until she is more stable before she explores her options.
“Why they tried to convince me I was a guy is the real mystery,” she said. “Because I wasn’t a normal guy, and I was bullied. Now I stand up to bullies.”
Wrexha has been homeless since she was a teenager. She exhibited behavioral issues in school and struggled with ADHD and bullying. Ultimately, her father forced her to leave the family home.
Wrexha sleeps where she can. She sees herself as a protector of women on the streets and still has a seething hatred of bullies. But one insect bite had immobilized her in pain, barely able to stand.
The injury lingered, but Wrexha refused to go to Denver Health and refused transportation to other clinics. She said that she has learned to be independent and find a way in impossible circumstances. “I’m not going to Denver Health,” she said. “They treat us like shit. I’ve had too many bad experiences there.”
Wrexha did get access to bandages and treatment and said that she hoped that her hand would heal without needing to go to a hospital or clinic.
Most people understand that in the event of extreme weather, people living unsheltered on the streets are at risk. But, like Wrexha, many also experience dangers and traumas that are hard to imagine.
Dr. Sarah Axelrath, a primary care and addiction medicine physician with the Colorado Coalition for the Homeless, said that the reality is far more complex and dangerous. Working through Stout Street Health Center’s clinics and street medicine teams, Axelrath treats people living outdoors across Denver. She describes a web of overlapping risks – medical, environmental, and social – that most people living in housing never have to think about.
“People who are unsheltered have higher rates of both acute and chronic illnesses and injuries,” she said. “We see a lot of acute injuries like accidental traumas, a lot of acute illnesses, like skin and soft tissue infections, and bad flus and pneumonias. And then we also see higher rates of pretty much every chronic medical condition you can name, including hypertension, diabetes, heart disease and cancers.”
Environmental risks and more traditional medical conditions often coexist, she said, compounding suffering and making treatment uniquely challenging.
Even when someone living on the streets wants treatment, accessing care can be difficult. “When you are homeless and unsheltered on the streets, you can’t just pick up and go to a doctor’s appointment,” Axelrath said. “They would have to potentially leave their tent unguarded with everything that they own inside. It’s like walking out of your front door with the door unlocked and wide open, inviting somebody in to steal everything you own.”
Barriers compound from there. Transportation and tracking appointment dates and times can be difficult when someone has few resources. And it is common for people experiencing homelessness to have deep trauma from past medical experiences, leading to distrust of medical institutions.
That fear and distrust, Axelrath said, is rooted in real harm. Many patients have been stigmatized or dismissed in emergency rooms and clinics, leaving them wary of returning even when their lives depend on it.
For those who live outdoors year-round, the environment itself can also be deadly. “We see a lot of frostbite in the winter, which leads to amputations and lifelong disability,” Axelrath said. “Then we see the opposite in the summer: heat stroke and heat exhaustion.”
People are also struck by cars or scooters, attacked, or fall ill from pollution and environmental hazards. “We see a lot of skin and soft tissue infections just because they don’t always have reliable access to basic hygiene,” Axelrath said. “It doesn’t take that much for something that starts as a mild infection to progress to something pretty bad.”
Respiratory illness is another recurring issue. “They’re inhaling smoke and exhaust fumes and staying in industrial areas [where they are less likely to be noticed] with dust or other chemicals,” Axelrath said.
Physical dangers often lead to emotional trauma, and the trauma itself feeds back into homelessness. One of the most misunderstood aspects of life on the streets, Axelrath said, is how trauma and fear can drive substance use. “Substance use as a cause of homelessness is not even in the top three,” she said. “The top causes are housing instability, unaffordability, and unemployment.”
But once people are on the streets, drug use often becomes a coping mechanism for extreme circumstances, Axelrath said. “Many people who are homeless did not use meth before they became homeless. They end up using meth during homelessness because they are trying to stay awake at night so they can be safe and not feel so vulnerable.”
That survival strategy can quickly trap people in a cycle of exhaustion and addiction. “There’s nowhere safe for them to sleep during the day,” she said, “so sometimes they use opiates to come down and try to get a little sleep. If they can’t, they use more meth to stay awake, and they get trapped in this cycle of profound sleep deprivation and escalating substance use.”
Traditional healthcare systems are rarely equipped to meet those realities. Many patients turn to emergency rooms, which provide only short-term solutions.
Street medicine and integrated outreach models are growing, Axelrath said, driven by younger healthcare workers eager to serve outside of traditional clinics. That gives her hope. “We could work anywhere else, but we all work here by choice because we think it’s important and we really
like doing it. That inspires me every day.”
For Axelrath, the goal is simple but urgent: meet people where they are, literally and emotionally, before the system fails them entirely.
Despite the agony of Wrexha’s injury, she insists that she has seen much worse on the streets. She knew a man who froze to death in a Porta Potty in Pueblo as he tried to survive a particularly cold night. “Someone has to die for things to change,” she said. “They finally opened the shelters [during extreme weather], but a man had to freeze to death.”
She paused, eyes heavy but fierce. “You’re gonna die in your sleep,” she imagined someone saying. “I won’t. I’m too powerful. I have trained and honed my body to be a fighting force, and that’s why I fight homelessness.”
Wrexha studies the swollen mark on her thumb, the scar left from the burrowing insect. For her, it is more than an injury – it is proof of what people outside endure unseen. “I can live out here and sleep in a yard and survive the cold night,” she said. “That’s all I need, thank you.”